Biological explanations and treatments
Biological Explanation: Genetic Factors
One possible explanation of schizophrenia may be heredity i.e. genetics. Schizophrenia tends to run in families, but only among individuals who are genetically related rather than related by marriage. The risk of developing the disorder among individuals who have family members with schizophrenia is higher than it is for those who do not. No one gene is thought to be responsible for this disorder – it’s more likely that different combinations of genes make individuals more vulnerable to schizophrenia. Having these genes does not necessarily mean an individual will develop schizophrenia.
Family Studies
Family studies have established that schizophrenia is more common among biological relatives of a person with schizophrenia, and that the closer the degree of genetic relatedness, the greater the risk.
For example, in Gottesman and Shield’s (1991) study, children with two schizophrenic parents had a concordance rate of 40%, children with one schizophrenic parent a rate of 12% and siblings (where a brother or sister had schizophrenia) a concordance rate of 9%.

Gottesman (2010) used a national register-based cohort study conducted in Denmark where around 75,000 participants were used. The IV = Parent diagnosed with schizophrenia or bipolar and the DV = Children diagnosed with any mental illness according to the International Classification of Diseases (ICD – 10)
Findings: The risk of being diagnosed with schizophrenia was much greater for offspring of two parents with a diagnosis – 27.3%. The risk increased when the calculation included offspring being diagnosed with other mental health issues – 67.5%. For offspring who had neither parent having any diagnosis, the risk was 1.1%
Twin Studies
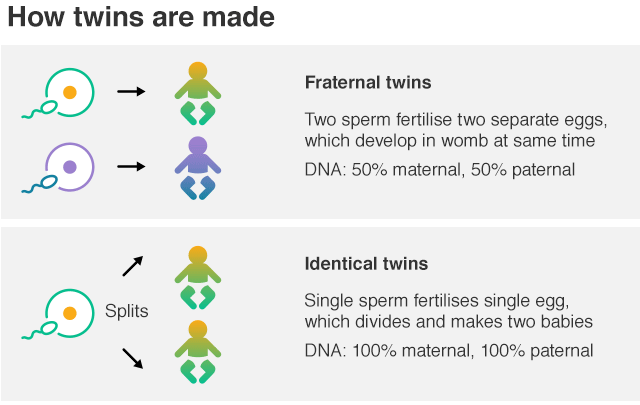
If monozygotic (MZ – genetically identical) twins are more concordant than dizygotic (DZ – who share only 50% of their genes), then this suggests that the greater similarity is due to genetic factors.
More evidence to support the genetic explanation comes from Gottesman and Shields, who found a concordance rate of 42% for MZ and 9% for DZ.
Adoption Studies
Because of the difficulties of disentangling genetic and environmental influences for individuals who share genes and environment, studies of genetically related individuals who have been reared apart are used.
Tienari et al (2000) found that of the 164 adoptees whose biological mothers had been diagnosed with schizophrenia, 6.7% also received a diagnosis of schizophrenia, compared to just 2% of the 197 controls adoptees (those born to non-schizophrenic mothers). The investigators concluded that these findings showed that the genetic liability to schizophrenia had been ‘decisively confirmed.’
Evaluation of genetic explanation
Strengths:
- Supporting research: There is overwhelming evidence to suggest that genetic factors make some people much more vulnerable to developing the disorder than others (see all research above). This does not mean that schizophrenia is entirely genetic. As outlined above there is research by: Gottesman and Shields, who found a concordance rate of 42% for MZ and 9% for DZ. Gottesman (2010) Offspring of two parents with a diagnosis of schizophrenia – 67.5% likelihood in developing some form of mental illness. Tienari et al (2000) found that in Finland, 164 adoptees whose biological mothers had been diagnosed with schizophrenia, 6.7% also received a diagnosis of schizophrenia, compared to 2% of the 197 controls adoptees (those born to non-schizophrenic mothers).
- Applications/Determinism: Understanding genetic vulnerabilities enable researchers to make predictions of mental illness. This deterministic view can help to direct early interventions, support, or treatment. You can use evidence from treatments that are stated at the bottom of this page.
Weaknesses:
- Alternative explanation – Nature/Nurture: There are a number of factors in the environment associated with risk of the disorder (which could account for concordance rates of less than 100%) and other research on expressed emotion (seen later) has shown that the negative emotional climate in some families may lead to stress beyond an individual’s coping mechanisms, thus triggering a schizophrenic episode.
- Issues with supporting research: Cause and effect may be difficult to establish with twin, family and adoption studies due to a lack of control, it is difficult to suggest that genetics is the only cause of schizophrenia. Use the Gottesman research for this point.
Biochemical explanation: The Dopamine Hypothesis
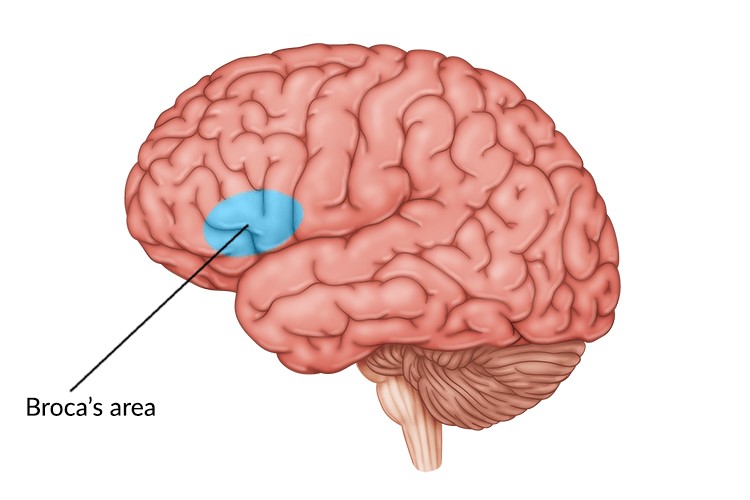
Hyperdopaminergia = Excessive levels of dopamine in the Broca’s area
The Broca’s area is responsible for speech production. Due to the excessive levels of dopamine, it it thought that speech poverty and auditory hallucinations could be linked.
Hypodopaminergia = Low levels of dopamine in the prefrontal cortex.
The prefrontal cortex is the right at the front of the frontal lobe. This brain region is thought to be responsible for planning complex cognitive behaviour and decision making. The basic activity of this brain region is considered to be orchestration of thoughts and actions in accordance with internal goals. Low dopamine activity could explain the symptoms of avolition as they find it difficult to initiate goal-directed behaviour.
Biostructure Explanation: Neural Correlates
Neural correlates are patterns of activity in the brain that occur with a schizophrenic experience. As they occur simultaneously, this could lead us to believe that the patterns observed are implicated in causing schizophrenia.

The superior temporal gyrus contains the auditory cortex, which is responsible for processing sounds. The anterior cingulate cortex (or ACC) has been implicated in several complex cognitive functions, such as empathy, impulse control, emotion, and decision-making. Allen et al (2007) scanned patients with auditory hallucinations, compared to a control. A negative correlation was found – lower neural activation levels were found in superior temporal gyrus and anterior cingulate gyrus and were correlated with an increase in positive symptoms such as auditory hallucinations.
The ventral striatum is thought to be responsible for the anticipation of rewards. Negative correlation between activity levels and severity of avolition. As neural activity decreases in the Ventral striatum, avolition symptoms increases.
Evaluation of dopamine explanation
- Supporting research: Allen et al (2007) scanned patients with auditory hallucinations, compared to a control. A negative correlation was found – lower neural activation levels were found in superior temporal gyrus and anterior cingulate gyrus and were correlated with an increase in positive symptoms such as auditory hallucinations.
- Useful Applications – Much of the evidence supporting the dopamine hypothesis comes from the success of drug treatments that attempt to change levels of dopamine activity in the brain. The basic mechanism of anti-psychotic drugs is to reduce the effects of dopamine and so reduce the symptoms of schizophrenia. Therefore, this explanation is useful in helping to develop treatments for schizophrenia. You can use evidence from the treatments section below.
- Reductionist – a simplistic explanation that is easy to explain to patients. Schizophrenia is a complex disorder with multiple neurotransmitter systems implicated. The dopamine hypothesis might oversimplify the intricate neural mechanisms involved in the disorder.
-
Inconsistencies in Dopamine Levels: Not all studies consistently find elevated dopamine levels in individuals with schizophrenia. This inconsistency raises questions about the reliability of dopamine dysregulation as the sole explanation. For example in the Allen study, not all participants will fit the correlation.
-
Deterministic – helps patients to realise that it is not their fault that they have this illness. Neurotransmitters are not something an individual can control, so it provides a sense of relief to the individual.
Biological Treatments for Schizophrenia
Anti-psychotics
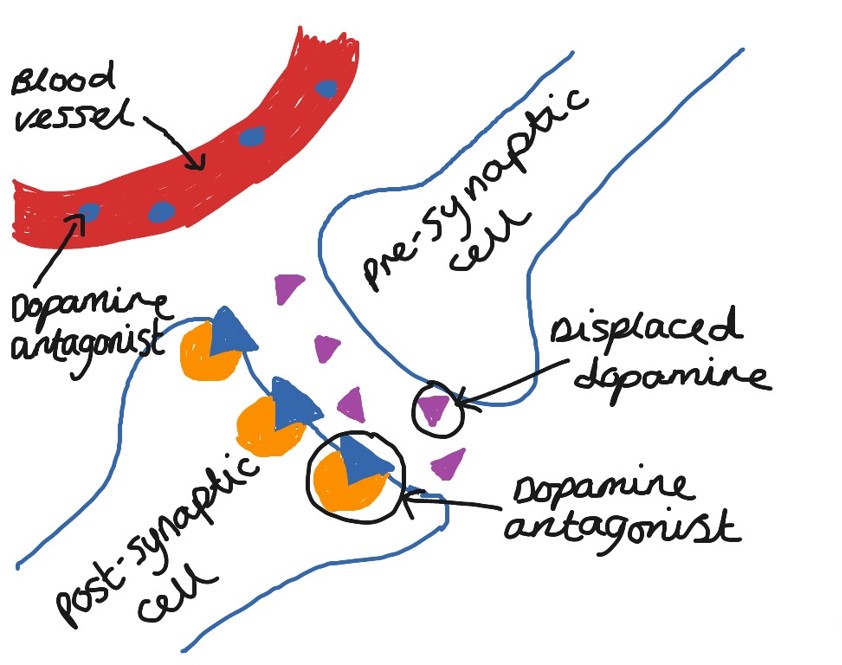
Anti-psychotics help the person with the disorder function as well as possible in their life, while at the same time increasing their feelings of subjective well-being. Anti-psychotics are usually recommended as the initial treatment for the symptoms of schizophrenia, after which clinicians will tend to use a combination of medication and psychological therapies. All anti-psychotics work by reducing dopaminergic transmission, i.e. reducing the action of dopamine in areas of the brain associated with schizophrenic symptoms.
- Typical antipsychotics (such as chlorpromazine) are used primarily to combat the positive symptoms such as hallucinations and thought disturbances, but doesn’t tend to work very well with negative symptoms.
- Atypical antipsychotics (such as clozapine) also combat these positive symptoms but they are also claimed to have some beneficial effects on negative symptoms as well.
Typical Anti-psychotics
Chlorpromazine pronounced as (klor pro ma zeen)– block the post synaptic dopamine receptors, which reduce the chances of dopamine being received. This reduces the effect of dopamine, and this is thought to be important due to schizophrenics having too much dopamine, or too many dopamine receptors. This has found to reduce positive symptoms such as hallucinations and is said to have a calming effect.
Typical anti-psychotics resulted in a high frequency of side effects. This problem has been addressed by the development of atypical anti-psychotic drugs which will cover next. Firstly, look over the side effects of typical anti-psychotics.
Typical Anti-psychotic side effects
Common side effects:
- dizziness
- drowsiness
- anxiety
- sleep problems (insomnia)
- breast swelling or discharge
- changes in menstrual periods
- weight gain
- swelling in hands or feet
- blurred vision
- constipation
- impotence or trouble having an orgasm
Serious long-term side effects:
- a movement disorder that may not be reversible. Extra-Pyramidal (movement) side effects (EPS) refers to our motor control and coordination. EPS is when you are unable to control motor movements. Examples include: restlessness and not being able to sit still, constant finger tapping, tremors and shakes – similar to Parkinson’s disease, uncontrollable facial movements or muscles involuntarily contract and contort.

-
Over blocking of dopamine in the hypothalamus can lead to a delirium, coma and even death! Some individuals died of this in the 1960’s when the drugs were first introduced. Nowadays, patients must take regular blood tests so that this can be monitored. If any issues are highlighted in the bloods, patients would not be prescribed the medication.
Atypical anti-psychotics
-
Clozapine works by blocking post synaptic dopamine receptors and post synaptic serotonin receptors. However, the atypical drugs only partially/weakly block the post synaptic dopamine receptors, therefore instead of cutting off dopamine on a large scale (like typical anti-psychotics), it still allows for some of the dopamine to be received.
- Serotonin is believed to help stabilize mood and have a calming effect. This is another reason why it is thought to improve negative symptoms more so than the Typical anti-psychotics. It is also believed that people with schizophrenia, may have higher levels of serotonin, so reducing the amount they are received may help to bring serotonin down to a normal level.
Atypical Common side effects:
- blurred vision
- confusion
- dizziness
- irregular heart beat
- fever
- sleepiness or unusual drowsiness
- sweating
- trembling or shaking of the hands or feet
Rare side effects:
- convulsions
- problems in urination
- hyperventilation
- loss of interest, pleasure or appetite
- muscle spasm or jerking of the arms or legs
- sudden loss of consciousness
- decreased sexual ability
Evaluation
Strengths:
- You only need to chose one of these studies to learn as research to support. Research to support – Thornley et al. (2003) reviewed studies on the drug treatments of schizophrenics by comparing groups who were taking Chlorpromazine to groups who were taking a placebo drug. Chlorpromazine was associated with better overall functioning, reduced symptom severity and fewer relapses in comparison to the placebo. Leucht et al (2012) carried out a meta-analysis of 65 studies published between 1959 and 2011, and involving nearly 6000 patients. All patients had been stabilised on either typical or atypical anti-psychotics. Some of these patients were taken off their medication and given a placebo instead. The remaining patients remained on there regular anti-psychotic. Within 12 months, 64% of those patients who had been given the placebo had relapsed compared to 27% of those who stayed on the anti-psychotic drug.
- Research to support effectiveness –Melter (2012) concluded that Clozapine is more effective than typical antipsychotics and is effective in 30-50% of treatment-resistant cases where typical antipsychotics have failed.
- Usefulness – Crossley et al (2010) carried out a meta-analysis for 15 studies to examine the efficacy and side effects of atypical drugs vs typical drugs in the early phase treatment of schizophrenia. Patients on atypical anti-psychotics gained more weight than those on typicals, whereas those on typicals experienced more extrapyramidal side effects. This could highlight the usefulness in terms of which drugs are more ethical. The usefulness of drug treatments should consider side effects, as if one form of drug has an increased risk in creating more problems in the individual than what they started with, this drug can be classed as more effective as a treatment.
Weaknesses:
- Usefulness: Research suggests that more than half of the patients taking typical anti-psychotics experience Parkison’s or extrapyramidal problems. These side effects can be so distressing for the patient that other drugs have to be given to control them, or the patient may stop taking their anti-psychotic medication.
-
Alternative explanation: Drug treatments are shown to be less beneficial when taken as a sole treatment. Tarrier et al. (2000) focused on people with schizophrenia receiving 20 sessions of CBT in 10 weeks. Those who participated in CBT and drugs had a better reduction in symptoms compared to those who were just taking drugs.
-
Lack of Freewill – Ross and Read (2004) argue that when people are prescribed anti-psychotic medication, it reinforces the view that there is ‘something wrong with them.’ This prevents the individual from thinking about possible stressors (such as life history or current circumstances) that might be possible for their condition. In turn this reduces their motivation to look for possible solutions that might alleviate these stressors and reduce their suffering. By taking a drug it takes away their freewill, this may make them feel out of control or that the treatment is being done to them. This could encourage a vicious cycle where individuals stop and start medication again and again.
